The Gut Microbiome: Understanding the Role of Bacteria in Digestion and Overall Health
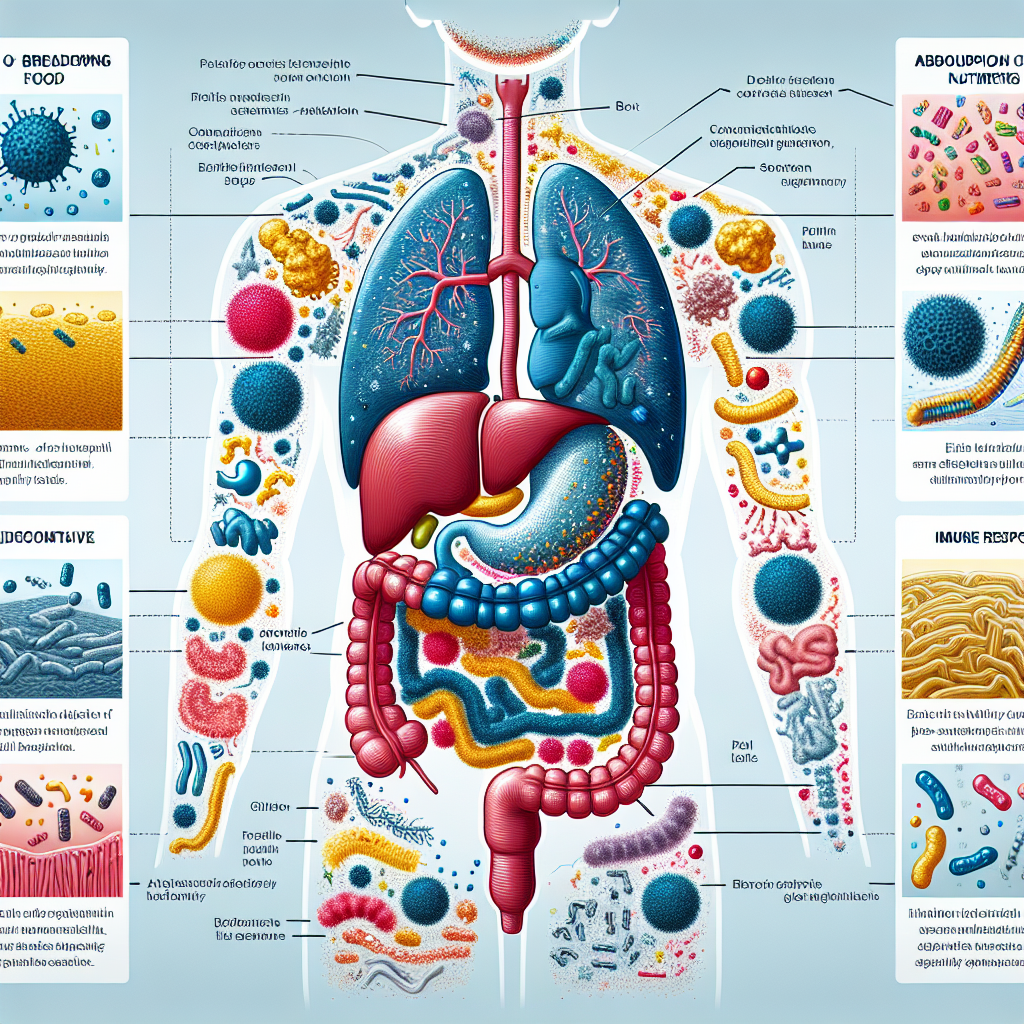
The gut microbiome refers to the trillions of microorganisms that reside in our digestive tract. These microorganisms, including bacteria, viruses, fungi, and other microbes, play a crucial role in maintaining our overall health. The gut microbiome is incredibly diverse, with hundreds of different species of bacteria alone.
The gut microbiome is important for several reasons. First and foremost, it helps with digestion and nutrient absorption. The bacteria in our gut break down complex carbohydrates, proteins, and fats that our bodies cannot digest on their own. They also produce vitamins and other essential nutrients that our bodies need.
In addition to digestion, the gut microbiome also plays a role in regulating our immune system. It helps to train our immune cells to recognize and respond appropriately to harmful pathogens, while also preventing them from attacking harmless substances. Furthermore, the gut microbiome has been linked to mental health, with research suggesting that imbalances in the microbiome may contribute to conditions such as anxiety and depression.
Key Takeaways
- The gut microbiome is a collection of microorganisms that play a crucial role in digestion, immune function, and mental health.
- Bacteria in the gut help break down food and extract nutrients that the body needs to function properly.
- The gut-brain connection is a complex relationship between the microbiome and the central nervous system that can affect mental health and mood.
- The microbiome also plays a key role in protecting against disease by interacting with the immune system.
- Imbalances in the microbiome, known as dysbiosis, can lead to a range of health problems, including digestive issues and chronic diseases.
The Role of Bacteria in Digestion: How Microbes Help Break Down Food
Bacteria are the most abundant microorganisms in the gut microbiome, with over 1,000 different species present. These bacteria help with digestion by breaking down complex carbohydrates, proteins, and fats that our bodies cannot digest on their own.
One way bacteria aid in digestion is through the production of enzymes. Enzymes are proteins that help speed up chemical reactions in the body. Bacteria produce enzymes that can break down complex carbohydrates into simpler sugars that our bodies can absorb and use for energy.
Bacteria also play a role in breaking down proteins. They produce enzymes called proteases that break down proteins into smaller peptides and amino acids. These smaller molecules can then be absorbed by the body and used for various functions such as building muscle and repairing tissues.
In addition to carbohydrates and proteins, bacteria also help with the digestion of fats. They produce enzymes called lipases that break down fats into fatty acids and glycerol. These smaller molecules can then be absorbed by the body and used for energy or stored as fat.
It is important to have a diverse microbiome because different species of bacteria have different functions and abilities. A diverse microbiome ensures that all types of food can be broken down and absorbed efficiently. Furthermore, a diverse microbiome is more resilient to disturbances and imbalances, which can help maintain overall gut health.
The Gut-Brain Connection: How the Microbiome Affects Mental Health
The gut-brain axis refers to the bidirectional communication between the gut and the brain. This communication occurs through various pathways, including the nervous system, immune system, and endocrine system. The gut microbiome plays a crucial role in this communication and has been shown to influence mental health.
Research has shown that imbalances in the gut microbiome, known as dysbiosis, may contribute to mental health disorders such as anxiety and depression. This is thought to occur through several mechanisms. First, the gut microbiome produces neurotransmitters such as serotonin, which is involved in regulating mood. Imbalances in the microbiome can lead to disruptions in serotonin production, potentially contributing to mood disorders.
Second, the gut microbiome interacts with the immune system, which plays a role in regulating inflammation in the body. Chronic inflammation has been linked to mental health disorders, and imbalances in the microbiome can lead to increased inflammation.
Furthermore, the gut microbiome produces metabolites that can cross the blood-brain barrier and directly affect brain function. These metabolites can influence neurotransmitter production, neuroinflammation, and other processes involved in mental health.
Research on the gut-brain connection is still in its early stages, but it holds promise for developing new treatments for mental health disorders. For example, interventions that target the gut microbiome, such as probiotics and dietary changes, have shown promise in improving symptoms of anxiety and depression.
The Immune System and the Microbiome: How Bacteria Protect Against Disease
| Topic | Data/Metrics |
|---|---|
| Immune System |
|
| Microbiome |
|
| Bacteria and Disease |
|
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens. The gut microbiome plays a crucial role in supporting the immune system and protecting against disease.
One way the microbiome supports the immune system is by training immune cells to recognize and respond appropriately to harmful pathogens. The bacteria in our gut help educate our immune cells, teaching them to distinguish between harmful pathogens and harmless substances. This helps prevent unnecessary immune responses and reduces the risk of autoimmune diseases.
Furthermore, the gut microbiome helps maintain a healthy balance of immune cells in the gut. Imbalances in the microbiome can lead to an overgrowth of harmful bacteria or a decrease in beneficial bacteria, which can disrupt the immune system and increase the risk of infections and other diseases.
Research has also shown that imbalances in the gut microbiome are associated with autoimmune diseases such as inflammatory bowel disease (IBD) and rheumatoid arthritis. In these conditions, the immune system mistakenly attacks healthy tissues in the body. Imbalances in the microbiome can trigger an inappropriate immune response, leading to chronic inflammation and tissue damage.
Understanding the relationship between the gut microbiome and the immune system is crucial for developing new treatments for autoimmune diseases. Therapies that target the microbiome, such as fecal microbiota transplantation (FMT) and probiotics, have shown promise in reducing inflammation and improving symptoms in patients with autoimmune diseases.
Dysbiosis and Gut Health: Understanding Imbalances in the Microbiome
Dysbiosis refers to an imbalance in the gut microbiome, where there is an overgrowth of harmful bacteria or a decrease in beneficial bacteria. Dysbiosis can occur due to various factors, including diet, stress, medications, and infections.
There are several causes of dysbiosis. One common cause is a poor diet that is high in processed foods, sugar, and unhealthy fats. These types of foods can promote the growth of harmful bacteria and decrease the diversity of the microbiome.
Stress is another factor that can contribute to dysbiosis. Chronic stress can disrupt the balance of bacteria in the gut and lead to imbalances in the immune system. This can increase the risk of infections and other diseases.
Medications, particularly antibiotics, can also disrupt the gut microbiome. Antibiotics are designed to kill harmful bacteria, but they can also kill beneficial bacteria in the process. This can lead to imbalances in the microbiome and increase the risk of infections and other complications.
Dysbiosis can have several effects on gut health. It can lead to digestive symptoms such as bloating, gas, diarrhea, and constipation. It can also increase the risk of infections, as harmful bacteria are able to overgrow and cause illness. Furthermore, dysbiosis has been linked to various chronic diseases such as obesity, diabetes, and inflammatory bowel disease.
Maintaining a healthy gut microbiome is crucial for overall gut health. This can be achieved through a balanced diet that is rich in fiber, fruits, vegetables, and fermented foods. Regular exercise, stress management techniques, and avoiding unnecessary antibiotic use can also help promote a healthy microbiome.
Diet and the Microbiome: How What You Eat Affects Your Gut Health

The gut-brain axis refers to the bidirectional communication between the gut and the brain. This communication occurs through various pathways, including the nervous system, immune system, and endocrine system. The gut microbiome plays a crucial role in this communication and has been shown to influence mental health.
Research has shown that imbalances in the gut microbiome, known as dysbiosis, may contribute to mental health disorders such as anxiety and depression. This is thought to occur through several mechanisms. First, the gut microbiome produces neurotransmitters such as serotonin, which is involved in regulating mood. Imbalances in the microbiome can lead to disruptions in serotonin production, potentially contributing to mood disorders.
Second, the gut microbiome interacts with the immune system, which plays a role in regulating inflammation in the body. Chronic inflammation has been linked to mental health disorders, and imbalances in the microbiome can lead to increased inflammation.
Furthermore, the gut microbiome produces metabolites that can cross the blood-brain barrier and directly affect brain function. These metabolites can influence neurotransmitter production, neuroinflammation, and other processes involved in mental health.
Research on the gut-brain connection is still in its early stages, but it holds promise for developing new treatments for mental health disorders. For example, interventions that target the gut microbiome, such as probiotics and dietary changes, have shown promise in improving symptoms of anxiety and depression.
Probiotics and Prebiotics: Supporting a Healthy Microbiome
Probiotics are live microorganisms that provide health benefits when consumed in adequate amounts. They are often referred to as “good” bacteria because they help promote a healthy balance of bacteria in the gut.
Probiotics can be found in various foods and supplements. Some common sources of probiotics include yogurt, kefir, sauerkraut, kimchi, and other fermented foods. Probiotic supplements are also available and can be taken daily to support a healthy microbiome.
Prebiotics are non-digestible fibers that serve as food for probiotics. They help promote the growth of beneficial bacteria in the gut. Prebiotics can be found in foods such as onions, garlic, bananas, asparagus, and whole grains.
Both probiotics and prebiotics have been shown to have several health benefits. They can help improve digestion, support a healthy immune system, reduce inflammation, and promote mental health. They may also help prevent and treat certain conditions such as diarrhea, irritable bowel syndrome (IBS), and inflammatory bowel disease (IBD).
It is important to note that not all probiotics and prebiotics are the same. Different strains of bacteria and types of fibers have different effects on the gut microbiome. Therefore, it is important to choose probiotics and prebiotics that are backed by scientific research and have been shown to be effective.
Antibiotics and the Microbiome: Understanding the Risks and Benefits
Antibiotics are medications that are used to kill or inhibit the growth of bacteria. They are commonly prescribed to treat bacterial infections such as strep throat, urinary tract infections, and pneumonia. While antibiotics can be life-saving in certain situations, they can also have negative effects on the gut microbiome.
Antibiotics work by targeting specific bacteria that cause infections. However, they can also kill beneficial bacteria in the process. This can lead to imbalances in the gut microbiome and increase the risk of infections and other complications.
Research has shown that antibiotics can disrupt the diversity and composition of the gut microbiome. This disruption can lead to an overgrowth of harmful bacteria, a decrease in beneficial bacteria, and an increase in antibiotic-resistant bacteria.
Furthermore, studies have shown that antibiotic use in early life can have long-term effects on the gut microbiome. This can increase the risk of various health conditions later in life, including obesity, asthma, allergies, and autoimmune diseases.
It is important to use antibiotics judiciously and only when necessary. This includes following the prescribed dosage and duration of treatment, as well as discussing any concerns or questions with a healthcare provider. In some cases, probiotics may be recommended alongside antibiotics to help support a healthy microbiome.
The Microbiome and Chronic Diseases: How Bacteria May Contribute to Illness
Research has shown that imbalances in the gut microbiome, known as dysbiosis, may contribute to the development of chronic diseases. Dysbiosis can lead to chronic inflammation, which has been linked to various conditions such as obesity, diabetes, cardiovascular disease, and inflammatory bowel disease.
In obesity, for example, imbalances in the gut microbiome have been observed. Studies have shown that obese individuals tend to have a less diverse microbiome compared to lean individuals. Furthermore, certain species of bacteria have been associated with obesity, with some bacteria being more prevalent in obese individuals.
Inflammatory bowel disease (IBD) is another condition that has been linked to dysbiosis. IBD is characterized by chronic inflammation of the digestive tract and includes conditions such as Crohn’s disease and ulcerative colitis. Imbalances in the gut microbiome have been observed in individuals with IBD, with a decrease in beneficial bacteria and an increase in harmful bacteria.
Autoimmune diseases such as rheumatoid arthritis and multiple sclerosis have also been linked to dysbiosis. In these conditions, the immune system mistakenly attacks healthy tissues in the body. Imbalances in the gut microbiome can trigger an inappropriate immune response, leading to chronic inflammation and tissue damage.
Understanding the role of the gut microbiome in chronic diseases is crucial for developing new treatments and interventions. Therapies that target the microbiome, such as fecal microbiota transplantation (FMT) and probiotics, have shown promise in reducing inflammation and improving symptoms in patients with chronic diseases.
Future Directions in Microbiome Research: Exploring New Therapies and Treatments
Microbiome research is a rapidly growing field, with new discoveries being made every day. Scientists are exploring new therapies and treatments that target the microbiome to improve health outcomes.
One area of research is the development of personalized medicine based on an individual’s microbiome. By analyzing a person’s gut microbiome, scientists can gain insights into their health and develop personalized treatment plans. This could include targeted probiotics, prebiotics, or dietary interventions to support a healthy microbiome.
Another area of research is the use of fecal microbiota transplantation (FMT) to treat various conditions. FMT involves transferring fecal matter from a healthy donor to a recipient to restore a healthy balance of bacteria in the gut. FMT has shown promise in treating conditions such as recurrent Clostridium difficile infection and inflammatory bowel disease.
Furthermore, researchers are exploring the use of engineered bacteria to deliver therapeutic molecules to the gut. This could include bacteria that produce specific enzymes or metabolites that can help treat certain conditions. For example, engineered bacteria could be used to produce neurotransmitters that can help regulate mood in individuals with mental health disorders.
Overall, continued research on the gut microbiome is crucial for understanding its role in health and disease. It holds promise for developing new therapies and treatments that can improve outcomes for a wide range of conditions. By supporting a healthy microbiome through diet, lifestyle changes, and targeted interventions, we can optimize our overall health and well-being.
If you’re interested in learning more about the impact of gut bacteria on our overall health, you might want to check out this article on “The Health Benefits of Choline and its Impact on Gut Bacteria” (link: https://healthydietdoctor.com/health-benefits-of-choline/). It delves into the role of choline in supporting liver health and brain function, as well as its potential benefits for gut bacteria. Understanding the connection between choline and gut health can provide valuable insights into how we can optimize our diet for a healthier microbiome.
FAQs
What are gut bacteria?
Gut bacteria are microorganisms that live in the digestive tract of humans and animals. They play a crucial role in digestion, immune system function, and overall health.
What is the importance of gut bacteria?
Gut bacteria are important for digestion, absorption of nutrients, and the production of vitamins. They also help to maintain a healthy immune system and protect against harmful bacteria.
How do gut bacteria affect mental health?
Gut bacteria can affect mental health by producing neurotransmitters and other chemicals that affect mood and behavior. They can also influence the immune system, which can impact mental health.
What factors can affect gut bacteria?
Factors that can affect gut bacteria include diet, antibiotics, stress, and age. A diet high in fiber and fermented foods can promote healthy gut bacteria, while antibiotics can disrupt the balance of bacteria in the gut.
Can gut bacteria be changed?
Yes, gut bacteria can be changed through diet, probiotics, and fecal microbiota transplantation (FMT). FMT involves transferring fecal matter from a healthy donor to a recipient to restore healthy gut bacteria.
What are the potential health benefits of healthy gut bacteria?
Healthy gut bacteria have been linked to a reduced risk of obesity, type 2 diabetes, heart disease, and certain types of cancer. They may also improve mental health and immune function.